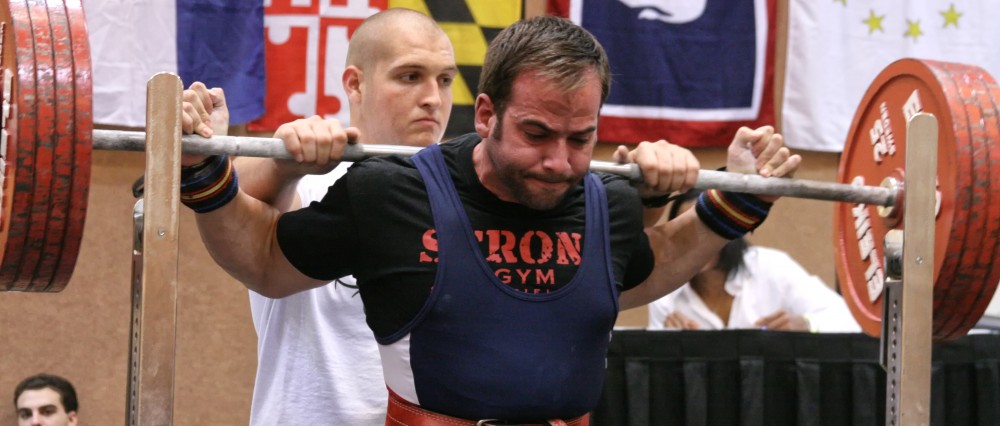
By Jordan Feigenbaum MS, Starting Strength Staff, CSCS, HFS, USAW CC
In case you missed part one of this three part series, click here. In today’s blog entry we’re going to talk about how alcohol affects skeletal muscle and the sex steroid, testosterone. Things can get pretty complicated in a hurry here, but what I aim to do is provide some basic science background for my readers as well as how a certain stressor, i.e. alcohol, can alter the internal milieu. I actually just used the words “internal milieu”, which describes the internal environment of the human body just so I could provide the following quote to pay homage to my previous physiology professors:
“The stability of the internal environment [the milieu intérieur] is the condition for the free and independent life”- Claude Bernard
The concept of the internal environment being important for physiological normalcy and a rationale for the human body’s homeostatic underpinnings was later expanded upon by Walter Canon’s characterization of homeostasis in 1932. He [Canon], proposed four characteristics of homeostasis as follows:
- Constancy in an open system, such as our bodies represent, requires mechanisms that act to maintain this constancy. Cannon based this proposition on insights into the ways by which steady states such as glucose concentrations, body temperature and acid-base balance were regulated.
- Steady-state conditions require that any tendency toward change automatically meets with factors that resist change. An increase in blood sugar results in thirst as the body attempts to dilute the concentration of sugar in the extracellular fluid.
- The regulating system that determines the homeostatic state consists of a number of cooperating mechanisms acting simultaneously or successively. Blood sugar is regulated by insulin, glucagons, and other hormones that control its release from the liver or its uptake by the tissues.
- Homeostasis does not occur by chance, but is the result of organized self-government.
It is important to appreciate the homeostatic mechanisms that the human body possesses in order to maintain an “even keel”, as without redundant pathways in place things can go awry in a hurry. At any rate, while the overall concept of the internal milieu and it’s influences on homeostasis are critically important, further discussion of it would preclude our look at just how alcohol/ethanol can alter skeletal muscle metabolism and testosterone levels. To begin, let’s talk a bit about skeletal muscle.
One of the most common effects of alcohol on striated muscle, i.e. skeletal and cardiac muscle, is fiber atrophy or reduction in size. Skeletal and cardiac muscle are both striated, as they have repeating sarcomeres and appear (under the microscope) to have alternating “light” and “dark” bands.
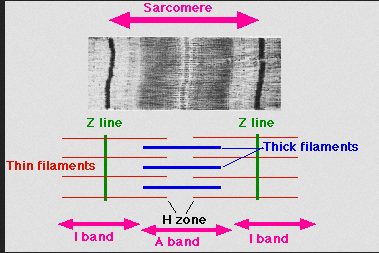 Smooth muscle on the other hand, which is found in lots of places like the walls of the vascular system and the GI tract, do not appear striated under a microscope because they lack the organized, repeating structure of the sarcomere.
Smooth muscle on the other hand, which is found in lots of places like the walls of the vascular system and the GI tract, do not appear striated under a microscope because they lack the organized, repeating structure of the sarcomere.
At any rate, striated muscle size is a result of the balance of protein synthesis and protein breakdown. In other words, the net flux of protein reflects the protein being built (synthesized) and deposited minus the protein being broken down and metabolized. If something were to either increase protein synthesis or inhibit (prevent) protein breakdown, their would be a net gain in protein levels. On the other hand, if the rate of protein breakdown is increased OR the synthesis of new protein is inhibited, there will be a net loss of protein. In general, a net gain of protein within muscle tissue results in hypertrophy (increased size) and a net loss of protein in the muscle tissue results in atrophy.
Ethanol tends to decrease striated muscle protein synthesis [1]. Interestingly, the resulting atrophy appears to be greatest in Type IIB fibers, which are a subtype of the fast-twitch muscle fibers that produce high amounts of force, contract rapidly, and are anaerobic. Some researchers actually classify type II muscle fiber atrophy as part of a diagnostic criteria of alcoholic myopathy, however this selective decrease in size also occurs in other issues like calorie malnutrition, neuropathy, etc. Additionally, only about 33% of chronic asymptomatic alcoholics show significant type II fiber atrophy without malnutrition, neuropathy, etc. although other studies report 40-60% of alcoholics presenting with significant atrophy [1]. Urbano et al. goes head to head with Preedy et al in the following quotes:
In fact, it [ethanol] is the most frequent cause of toxicity to striated skeletal and cardiac muscle in adults in dose dependent fashion [1].
“Due to the ethanol-induced reduction of muscle phosphorylase activity, decreased rates of protein synthesis and whole-body protein metabolism by 15–30%, predominantly in type II fast-twitch anaerobic fibers that utilize glycolytic metabolism.Type I fibers were not overly affected and there was no clear decrease in muscle protein breakdown [5].
As far as how this occurs on a cellular level, it appears as though ethanol consumption disrupts the translation of would-be muscle-protein RNA, but not it’s transcription. For background information, muscle protein synthesis signalers (like eating a protein-rich meal or training) increase the transcription of certain DNA to muscle protein RNA. Muscle protein RNA is then translated into muscle protein, which is shuttled to it’s target and deposited as muscle. Through increased binding of a variety of different regulatory sites on the muscle protein RNA, translation is decreased and total muscle protein synthesis decreases [2].
Measuring decreases in total muscle protein synthesis can be tricky in the laboratory settings, as most of the time a total nitrogen balance measurement is used. Remember, protein is the only macronutrient with nitrogen as a component. Therefore, it intuitively makes sense that the amount of nitrogen taken in minus the amount of nitrogen excreted can give insight into the nitrogen balance of a person or animal. Unfortunately, some people take this sort of information as definitive with regards to what is actually happening in the muscle specifically. Remember, all tissues (lungs, gut, kidney, visceral organs, etc.) are made up of protein, which are also turned over regularly and thus influence total body protein and nitrogen balance. Lang et. al. provide a nice quote describing this:
However, whole body measurements represent the sum of many vastly different organ systems (e.g., muscle and nonmuscle protein synthesis and hepatic secretory protein synthesis) and provide little information concerning individual processes or tissues.
So while total body nitrogen balance tells us what’s happening on a body wide or systemic level, it does not tell us what’s happening in just the muscle tissue. Muscle protein turnover, in sum, makes up less than 30% of total body protein turnover anyway [3]. Other studies, however, have shown that with acute alcohol intoxication muscle protein synthesis decreases in skeletal muscle, heart, intestine, bone, and skin. Additionally, chronic ethanol exposure has been demonstrated to decrease skeletal muscle protein synthesis in rats [4, 5]. It appears that ethanol exposure is potentially harmful to overall protein synthesis, as described in the following quote:
“However, experimental and clinical studies have clearly demonstrated that ethanol itself is a direct noxious agent to heart and skeletal muscle in a progressive, cumulative, and dose-dependent manner, an effect independent of nutritional, vitamin, or mineral factors.”-[Nguyen et al. (6)]
There are only a couple of things left to discuss with respect to actual skeletal muscle function and ethanol. First, muscle glycogen concentration tends to increase in chronic alcohol patients because glycogen cannot be degraded as efficiently. This is due to a partial inhibition of the biochemical pathway for glycogenolysis (glycogen breakdown) as well as glycolysis (glucose breakdown) [5]. In contrast, acute alcohol exposures tend to decrease glycogen storage, especially post workout as some of the mechanisms used to store glycogen in skeletal muscle are inhibited and instead fatty acid production is increased. These effects are independent of acetaldehyde toxicity, which was discussed in part one of this series [5].
Ethanol and acetylaldehyde also tend to increase formation of reactive oxygen species due to their effects on vitamin metabolism. Reactive oxygen species (ROS) tend to increase cellular damage and stress in the skeletal muscle, thus increasing damage to cells of the muscles which may increase atrophy.
Moving along, let’s start our discussion about alcohol and testosterone production by covering the general overview of testosterone production in vivo (in the body). This will give us some background to what is normal so we can consider the effects of ethanol on the internal milieu and homeostasis.
 Normally, males produce testosterone in the Leydig cells of the testes from cholesterol via increasing leutinizing hormone (LH) activity within the testes. LH increases an enzyme called cholesterol desmolase, which is responsible for converting cholesterol to pregnenolone. Pregnenolone will go on to be converted through various enzymes to testosterone and thus, but first it needs to be formed from cholesterol. Thus, increasing the enzymatic activity of cholesterol desmolase helps to increase testosterone production.
Normally, males produce testosterone in the Leydig cells of the testes from cholesterol via increasing leutinizing hormone (LH) activity within the testes. LH increases an enzyme called cholesterol desmolase, which is responsible for converting cholesterol to pregnenolone. Pregnenolone will go on to be converted through various enzymes to testosterone and thus, but first it needs to be formed from cholesterol. Thus, increasing the enzymatic activity of cholesterol desmolase helps to increase testosterone production.
Naturally, one would ask well what increases LH? Gonadotropin releasing hormone (GnRH) is secreted by the hypothalamus in the brain. GnRH is released into blood vessels that carry this peptide to the anterior pituitary gland (hypothalamic-hypophysial portal system). GnRH is normally secreted in a pulsatile fashion, i.e. it is not constant. It acts on certain cells in the anterior lobe of the pituitary gland (gonadotropes) to cause them to manufacture and release LH, which is also released in a pulsatile fashion. LH is released into the systemic (body-wide) circulation where it ends up traveling to the testicles and causing the Leydig cells to pump out testosterone, as described above.
As discussed at the beginning of this post, most, if not all of the body’s pathways are tightly regulated to keep it on an “even-keel”. Let’s explore this now that we know the testosterone-producing pathway. Testosterone produced by the Leydig cells provides what’s known as “negative feedback” on the hypothalamus and cells of anterior lobe of the pituitary, effectively decreasing secretion of GnRH and LH. Thus, when testosterone levels are high, GnRH and LH levels are low. Conversely, when testosterone levels are low, the frequency and amplitude of GnRH pulses are increased. A downstream effect of this is increased LH release and thus, increased signaling to the Leydig cells to produce more testosterone because the negative feedback signaling is removed.
As we’ll see in the upcoming discussion of ethanol’s effects, perturbation at any level of this pathway can result in deleterious effects. So, how does ethanol affect testosterone production and/or signaling?
As it turns out, ethanol exposure appears to lower GnRH levels, which leads to reduced LH secretion from the anterior pituitary and reduced testosterone production by the Leydig cells of the testes [7]. Mechanistically, this occurs because a hormone normally produced in the testes and hypothalamus at very low levels, β-endorphin (an endogenous opiod), normally only slightly suppresses testicular testosterone production and release. In the hypothalamus, β-endorphin results in decreased GnRH release. Adams and Cicero have shown an increase in β-endorphin after acute alcohol exposure [10]. Naltrexone, a treatment currently used in alcoholism to decrease alcohol cravings, blocks B-endorphin activity and may prevent reduced testosterone levels. Three other ways ethanol affects active GnRH levels is through acetalaldehyde, which is toxic, disturbing nerve impulses outside the hypothalamus that signal GnRH production WITHIN the hypothalamus, and finally, ethanol appears to interfere with processing of the inactive GnRH precursor to the active GnRH form according to Uddin et al.
LH levels actually decrease with alcohol exposure, which is not what we’d expect. Harkening back to our homeostatic mechanism discussion, if testosterone production falls, we’d expect GnRH and LH levels to increase to “right the ship”. However, as discussed above GnRH levels actually decrease and so do LH levels. Mechanistically, the decreased LH levels appear to be due to the toxic affect of ethanol directly on the anterior pituitary gland where LH is released by interfering with GnRH’s signaling of LH production in the cells that they act on (gonadotropes). Another effect of ethanol on LH that causes it’s decrease is that alcohol in the blood tends to result in the anterior pituitary gland’s production of less potent LH variants, thus decrease the level of LH in the blood and the quality of LH in the blood too.
A study done by Steiner and colleagues in 1996 found that when males were given a 15-percent alcohol solution that was administered every 3 hours, around the clock, together with a diet replete with protein, vitamins, folic acid, and minerals (total daily alcohol dose was 220g or 3g/kg body weight, which equals 15 drinks) that the testosterone levels in the men’s blood declined 5 days into the study and continued to fall over the entire period. This was attributed to a decrease in testosterone production in the Leydig cells of the testes and increased removal rate of testosterone from the blood via catabolic processes. On the other hand, Southren et al. found that the increased testosterone catabolism or breakdown is only present in men without liver disease, whereas the clearance is decreased in men with liver disease.
Numerous studies in human and animal models have since confirmed reduction in testosterone levels after either acute or long term alcohol exposure. Acute alcohol ingestion appears to result in a significant reduction in testosterone levels that lasted for 96 hours in a rat model [9].
Sarkola and Eriksson actually found that testosterone can increase in men exposed to a low dose of ethanol, although this is a transient effect due to the predomination of decreased liver clearance of testosterone from the blood compared to the decreased testosterone production in the testes. Unfortunately, during the latter stages of elimination of alcohol or when alcohol has been completely eliminated, testosterone production decreases even more. Similarly, in higher doses of alcohol consumption, e.g. 1.5g/kg, the decreased production of testosterone predominates over the transient decreased clearance rate of testosterone. This has been confirmed by experiemental evidence from Välimäki et al in 1990 and Ylikahri et al. in 1974 [10].
Another interesting finding is that alcohol abuse and subsequent impaired testosterone production tends to result in testicular atrophy/shrinkage, which occurs in about 75% of men with advanced cirrhosis [10]. The atrophy most likely results from the toxicity on the testes, decreased LH and FSH production, and other confounding factors causing decreased sperm cells and sperm production.
Finally, and perhaps one of the more important ways alcohol effects testosterone’s activity and blood levels is that ethanol exposure tends to increase aromatization of testosterone and testosterone precursors. Aromatase is an enzyme that converts testosterone to estrogen and thus, increased aromatization results in increased conversion of testosterone to estrogen. Additionally, the immediate precursors to testosterone, androstenedione (Mark McGwire?) can be “aromatized” to another estrogen subtype called estrone. Scientific evidence points to this “increased aromatization” as a byproduct of increased estrogen production and not a decrease in estrogen clearance [10]. Aromatization is not a good thing above physiological normal (homeostatic) levels in men, as the authors conclude:
“In addition to causing breast enlargement, estrogens appear to exert a negative feedback effect on LH and FSH production and may thereby contribute to alcohol’s suppression of those key reproductive hormones.”
While alcohol certainly has some benefits, which we’ll get to I PROMISE, it’s important to know the deleterious effects that alcohol can have on the internal milieu, especially as it pertains to training. Again, I’ll leave you with my favorite axiom related to alcohol consumption and training:
“If you’re drinking enough to get drunk, you’re drinking enough to mess with your results.”
Until next time.
-thefitcoach
1) Urbano-Marquez, A.; Fernandez-Sola, J. Effects of alcohol on skeletal and cardiac muscle. Muscle Nerve 2004, 30, 689-707.
2) Lang, CH, Wu, DQ, Frost, RA. Inhibition of muscle protein synthesis by alcohol is associated with modulation of eIF2B and eIF4E. American Journal of Physiology-Endocrinology and Metabolism 1999, 277, 268-276.
3) White JP, Baynes JW, Welle SL, Kostek MC, Matesic LE, et al. (2011) The Regulation of Skeletal Muscle Protein Turnover during the Progression of Cancer Cachexia in the ApcMin/+ Mouse. PLoS ONE 6(9)
4) Preedy V. R.,Peters T. J.,Patel V. B.,Miell J. P. (1994) Chronic alcoholic myopathy: transcription and translational alterations. FASEB J. 8:1146–1151
5) Preedy V. R., Peters T. J. (1990) Changes in protein, RNA, DNA and rates of protein synthesis in muscle-containing tissues of the mature rat in response to ethanol feeding: a comparative study of heart, small intestine and gastrocnemius muscle. Alcohol Alcohol. 25:489–498.
6) Nguyen VA, Le T, Tong M, Silbermann E, Gundogan F, de la Monte SM. Impaired Insulin/IGF Signaling in Experimental Alcohol-Related Myopathy. Nutrients. 2012; 4(8):1058-1075.
7) Vatsalya Vatsalya, Julnar E. Issa, Daniel W. Hommer, and Vijay A. Ramchandani. Pharmacodynamic Effects of Intravenous Alcohol on Hepatic and Gonadal Hormones: Influence of Age and Sex. Alcohol Clin Exp Res. 2012 February; 36(2): 207–213.
8) Sarkola, T. and Eriksson, C. J. P. (2003), Testosterone Increases in Men After a Low Dose of Alcohol. Alcoholism: Clinical and Experimental Research, 27: 682–685
9) Steiner, J., Halloran M.M., Jabamoni K., Emanuele, N.V., Emanuele, M.A. Sustained effects of a single injection of ethanol on the hypothalamic-pituitary-gonadal axis in the male rat. Alcoholism: Clinical and Experimental Research 20:1368–1374, 1996.
10) Emanuele, N.V., Emanuele, M.A. (1998) Alcohol’s Effects on Male Reproduction. The Alcohol and Other Drug Thesaurus. Vol. 22, No.3.